Table of Contents
Ozempic is a prescription medication used to improve blood sugar management in adults with type 2 diabetes and to support healthy weight reduction. Its active ingredient, semaglutide, is part of the GLP-1 receptor agonist class, medications that act like a natural hormone involved in regulating blood sugar and appetite. These effects help address two major challenges in type 2 diabetes: elevated glucose levels and difficulty maintaining a balanced eating pattern. This information is educational only; a healthcare professional should guide personal treatment decisions.
What Ozempic Is and How It Is Used
Ozempic is a once-weekly injectable medication developed by Novo Nordisk and approved in 2017 for adults with type 2 diabetes. It is designed for long-term use alongside diet and physical activity.
Although its main approval is for diabetes, some healthcare providers prescribe it off-label for weight management when clinically appropriate.
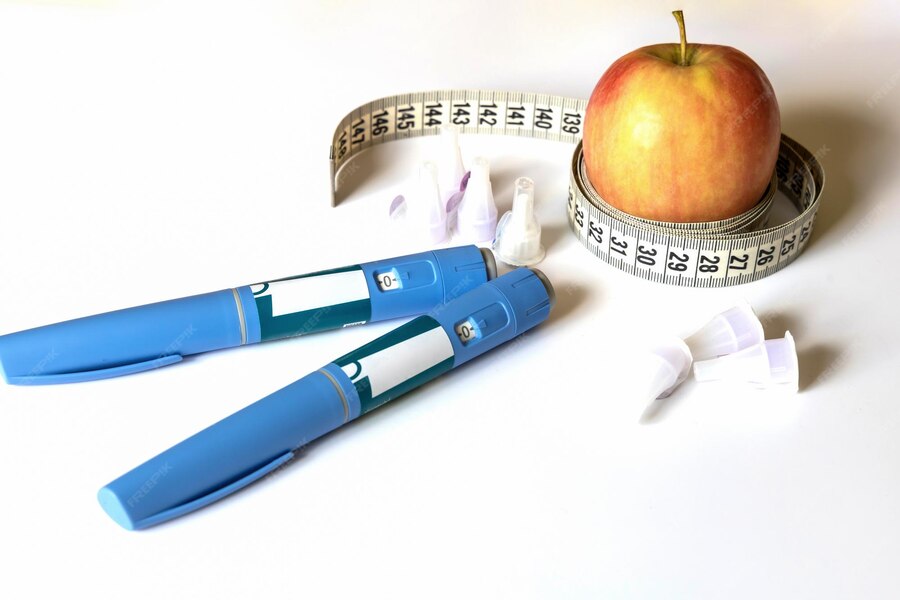
The medication comes in a prefilled pen and is injected under the skin of the abdomen, thigh, or upper arm. Weekly dosing makes it practical for everyday life, and the pen design supports consistent use.
How GLP-1 Receptor Agonists Work
GLP-1, short for glucagon-like peptide-1, is a hormone released after eating. It helps regulate appetite, blood sugar, insulin secretion, and digestion. In type 2 diabetes, GLP-1 signaling may not function normally, which can contribute to elevated blood glucose and increased hunger.
Semaglutide is a long-acting version of GLP-1. While natural GLP-1 breaks down within minutes, semaglutide remains active for about a week. This extended activity allows Ozempic to deliver steady effects on appetite, digestion, and glucose control.
Dosing and Titration
Ozempic doses increase gradually so the body can adjust comfortably.
- Weeks 1 to 4: 0.25 mg once weekly
- Week 5 onward: typically increased to 0.5 mg
- Higher doses such as 1 mg or 2 mg may be used depending on response
Slow titration helps minimize nausea and other gastrointestinal side effects as the medication becomes more active.
How Ozempic Supports Blood Sugar Control
Blood sugar regulation is at the center of Ozempic’s role in type 2 diabetes. It works through several complementary mechanisms.
1. Stimulating Insulin Release When Needed
Ozempic increases insulin secretion from the pancreas only when blood sugar is elevated. This glucose-dependent action helps lower post meal blood sugar without causing unnecessary drops.
2. Reducing Glucagon Levels
Glucagon is the hormone that signals the liver to release stored sugar. Ozempic lowers glucagon levels when blood sugar is high, helping prevent excess glucose from entering the bloodstream.
3. Slowing Gastric Emptying
Food leaves the stomach more slowly under the influence of semaglutide. This reduces the rate at which carbohydrates enter the bloodstream and results in gentler, more predictable glucose curves throughout the day.
Clinical trials show A1C reductions of 1.0 percent to 1.8 percent depending on the dose and baseline levels.
4. Evidence from the SUSTAIN Clinical Trials
In the large SUSTAIN program, thousands of participants using Ozempic achieved significantly better glycemic control than those on placebo or certain other diabetes treatments. Many reached an A1C below 7 percent, which is a standard goal in diabetes care. These benefits persisted with continued use, supporting Ozempic as a stable long-term option.
How Ozempic Suppresses Appetite
Alongside blood sugar benefits, Ozempic influences appetite and food intake in ways that support meaningful weight reduction.
1. Acting on the Brain’s Appetite Centers
Semaglutide reaches GLP-1 receptors in the hypothalamus, the area of the brain that helps regulate hunger and fullness. Activation of these receptors promotes a sense of satiety and helps reduce cravings, especially for calorie-dense foods.
2. Enhancing Fullness Through Delayed Digestion
Because Ozempic slows the movement of food out of the stomach, people feel full for longer after meals. This helps naturally reduce portion sizes and snacking without rigid dieting.
3. Encouraging Healthier Eating Patterns
Many people notice a s15ift toward smaller meals and more nutritious choices. This behavioral change plays a major role in lasting results and supports overall metabolic health.
4. Weight Loss Data from STEP Trials
In the STEP clinical trials, semaglutide consistently supported 15 percent to 20 percent body weight reduction over 68 weeks among adults with obesity or overweight. These results were largely driven by reduced energy intake due to improved appetite regulation.
Synergy Between Blood Sugar and Appetite Effects
Ozempic’s actions reinforce each other in a helpful cycle.
- Stable blood sugar reduces fatigue and cravings
- Eating less improves insulin sensitivity
- Better insulin sensitivity enhances blood sugar control
These combined effects explain why semaglutide has become a key tool in metabolic health.
Additional Health Benefits
Beyond blood sugar and weight control, Ozempic may support cardiovascular health by reducing the risk of major events such as heart attack or stroke in adults with type 2 diabetes and known heart disease. Weight reduction can also improve cholesterol, blood pressure, and inflammation markers.
Common Side Effects and How to Manage Them
Gastrointestinal symptoms are the most frequent side effects, especially nausea, vomiting, diarrhea, or constipation. Up to 44 percent of new users experience mild GI issues during early weeks.
Helpful strategies include:
- Eating small, simple meals
- Staying hydrated
- Avoiding heavy, greasy, or very sweet foods
Symptoms usually lessen as the body adjusts.
Low blood sugar is uncommon with Ozempic alone but can occur when combined with other glucose-lowering medications.
Who Benefits Most from Ozempic
Ozempic is typically used for:
- Adults with type 2 diabetes whose blood sugar is not controlled through diet, exercise, or oral medications
- People with excess weight and metabolic risk factors when clinically appropriate
It is not approved for:
- Type 1 diabetes
- People with a personal or family history of certain thyroid cancers
- Individuals with specific medical contraindications
Starting Ozempic and Monitoring Treatment
A healthcare professional evaluates eligibility, medical history, and treatment goals. Telehealth services have made this process more accessible for many people.
Routine monitoring includes:
- A1C
- Blood sugar patterns
- Side effect evaluation
- Dose adjustments as needed
Long-term success usually involves consistent medication use, healthy eating habits, and regular physical activity.
Frequently Asked Questions About How Ozempic Works
Does Ozempic lower blood sugar immediately?
Its effects begin within the first week, but full benefits appear gradually as the dose increases and the body adjusts.
Why does Ozempic reduce appetite?
Semaglutide activates GLP-1 receptors in brain regions that control hunger, and it also slows digestion. Both actions contribute to feeling full sooner and staying full longer.
Can Ozempic cause low blood sugar?
Ozempic rarely causes low blood sugar on its own because it stimulates insulin only when blood sugar is elevated. The risk increases if used with certain other diabetes medications.
How fast do people lose weight on Ozempic?
Weight loss is gradual. Most people notice changes over several weeks, with larger reductions occurring over several months as appetite decreases and eating patterns shift.
Does slowing digestion make Ozempic unsafe?
Delayed gastric emptying is expected and helps control blood sugar and appetite. Some people experience nausea at first, but this often improves as the body adapts.
Can someone without diabetes take Ozempic?
Its official approval is for type 2 diabetes. Some providers prescribe it off-label for weight management when medically appropriate.
Conclusion
Ozempic supports type 2 diabetes management by stabilizing blood sugar, improving insulin response, and reducing unnecessary glucose release. At the same time, it helps regulate appetite and eating behavior through effects on digestion and the brain’s satiety centers. These combined actions offer a balanced and effective approach to metabolic health when used under medical guidance.